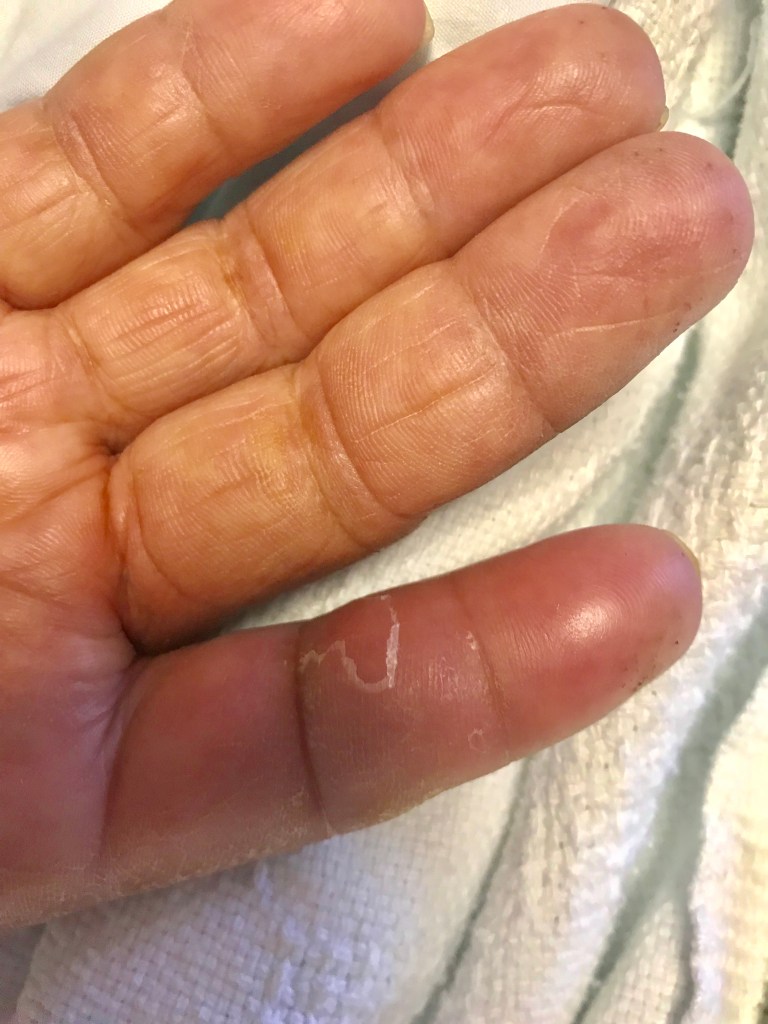
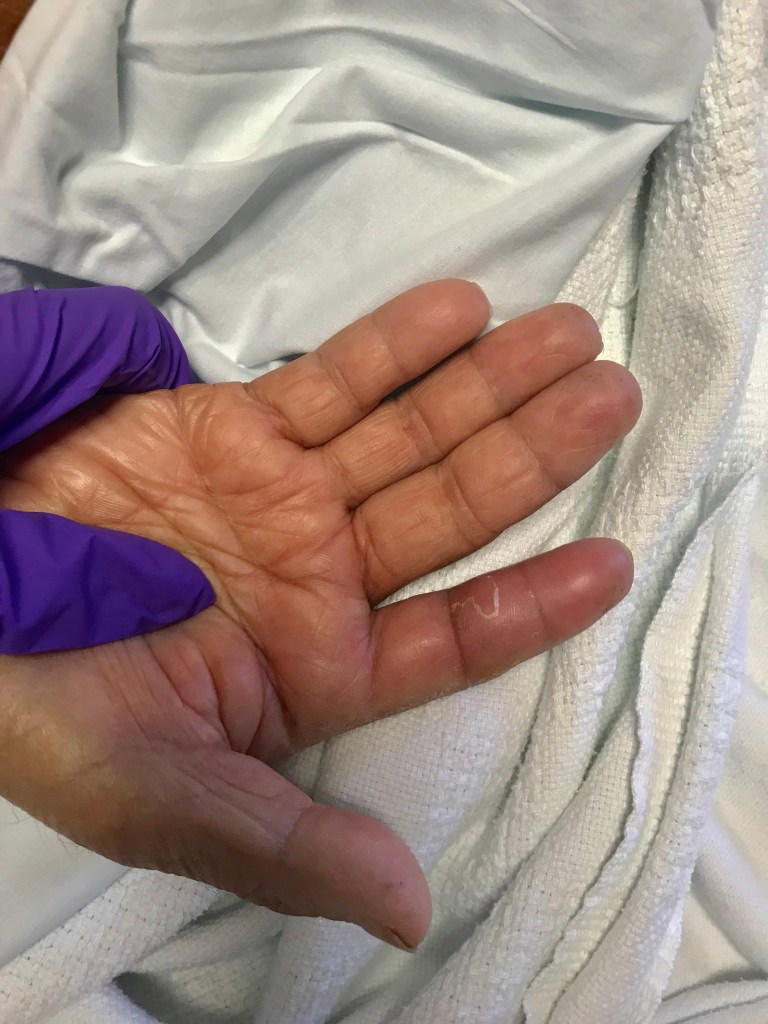
Case: A middle-aged gentleman with a history of kidney transplant presented with a painful swollen right index finger. The pain and swelling started the day before. There was no preceding trauma to the finger. On exam, fusiform swelling of the digit, tenderness along the flexor tendon sheath, and extreme pain with passive extension of the finger was noted. Orthopedic surgery was consulted. The patient was taken to the OR where a diagnosis of pyogenic flexor tenosynovitis was confirmed.
Diagnosis: pyogenic flexor tenosynovitis
Physical exam signs: This patient presented with three out of four Kanavel signs, which were strongly suggestive of pyogenic flexor tenosynovitis. Dr. Kanavel was a hand surgeon from the early 1900s who worked at Cook County Hospital in Chicago, Illinois. He made the following observation:
“The fingers are all slightly flexed. Now, how shall the differential diagnosis be made? Press deeply and firmly in all parts of the hand and fingers; the patient will volunteer the information that all points hurt; but if the tendon sheath is involved, pressure upon it throughout its course causes an immediate and involuntary expression of pain, and while before the patient has allowed his hand to remain passive in yours, he will now attempt to withdraw it voluntarily, and there is no doubt in your mind of the exquisite tenderness over this area. If the tenderness is outlined by the extent of the sheath, your diagnosis is nearly made. As a matter of fact, the greatest tenderness is generally complained of on deep pressure at the proximal end of the finger sheaths in the palm of the hand, just over the metacarpophalagneal articulation.”
The four Kanavel signs are:
- Fusiform swelling of the digit
- Slight resting flexion of the digit
- Tenderness along flexor tendon sheath of the digit
- Pain with passive extension of the digit
Kanavel signs were validated as being highly sensitive (>94% for each individual sign) and moderately specific in differentiating PFT from other diagnoses in patients with suspected hand infections (51 – 69%). Another significant differentiator was duration of symptoms less than 5 days.
It is important to understand that the deep spaces of the hand can be refractory to antimicrobial therapy alone and can rapidly progress up the arm, therefore when PFT is suspected based on physical examination, urgent orthopedic surgical consultation should be pursued. Do not wait to confirm the diagnosis with CT or MRI! Ideally, the diagnosis should be confirmed intraoperatively to avoid time delay and increased morbidity and mortality. Check out this NEJM case, “Just a Cut,” outlining a fulminant case of PFT due to Vibrio spp in a patient on anti-TNF (adalimumab) for psoriatic arthritis (https://www.nejm.org/doi/full/10.1056/NEJMcps1512793). Take note of the deep spaces of the hand, which communicate with each other and facilitate rapid proximal spread of infection.
The most common pathogens causing PFT are skin flora such as Staph spp, Strep spp, but its important to keep in mind patient-specific factors that might influence your microbial differential diagnosis. These factors include nosocomial exposure (MRSA, nosocomial GNRs such as Pseudomonas), water exposure (Vibrio, Aeromonas, etc.), diabetes (polymicrobial, GNRs), immune suppression (fungal organisms), animal bites (polymicrobial, staph aureus, Pasteurella multocida), plant thorns (fungal), or subacute presentations (more indolent organisms, fungal, NTM).
Treatment of PFT involves prompt administration of appropriate intravenous antimicrobial therapy based on patient-specific risk factors as defined above and prompt involvement of orthopedic surgery. Some mild cases can be treated non-surgically, but typically this is considered a surgical disease so prompt surgical assessment is imperative. In severe cases, don’t wait for an MRI, consult hand surgery to make the diagnosis in the OR to avoid the possibility of limb loss!